Renin-Angiotensin-Aldosterone
System (RAAS)
·
Function: maintain blood volume, BP,
and total body Na.
·
RAS → renal hypoperfusion → activation
of RAAS → vasoconstriction, and volume expansion.
·
Continous activation of the RAAS → changes of
heart and vessels.
·
Renin is a proteolytic enzyme that is
released from the granules of the juxtaglomerular apparatus (JGA) by ↓
pressure of afferent arteriole.
·
Renin converts angiotensinogen → angiotensin
I.
·
angiotensin-converting enzyme (ACE) convert
angiotensin I → angiotensin II.
·
angiotensin II: very potent
vasoconstrictor.in plasma, kidney, heart, lung and brain.
·
Angiotensin II →
Ø release
of aldosterone from the adrenal cortex, → Na reabsorption (salt&water
retention) and K excretion in DCT.
Ø activates
the G-protein coupled receptor angiotensin type 1 receptor (ATR1) → V.C.,
upregulation of other endogenous vasoconstrictors, and ↑ Na absorption by
the kidney.
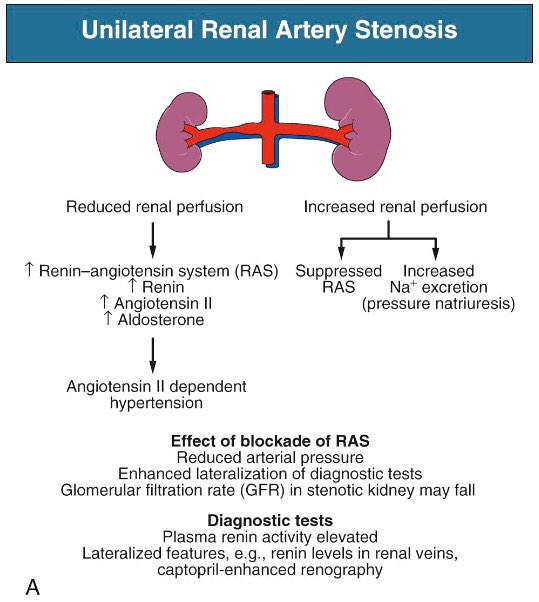
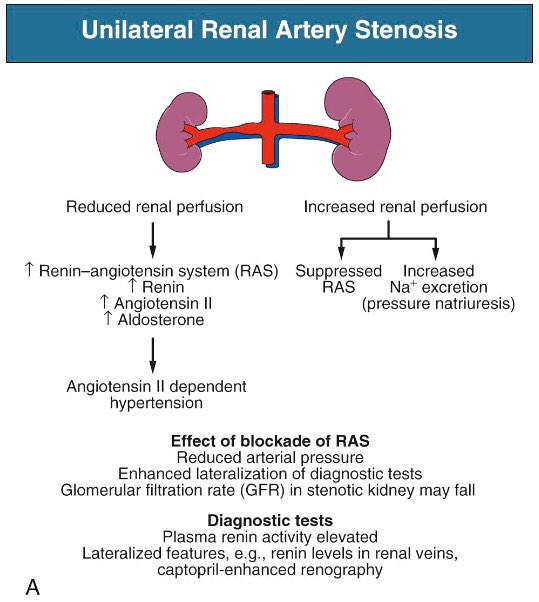
Mechanism of RVH:
1.
V.C. (Angiotensin II): unilateral RAS.
2.
Volume expansion (Aldosterone): Bilateral
or solitary kidney RAS.
·
Models:
1.
Unilateral RAS → contralateral kidney ↓
Na and water absorption (compensatory mechanism for the diseased kidney) → ↓
volume expansion. HTN is due to Angiotensin II (Vasoconstrictor
–Hypertensive model)
2.
Bilateral or solitary kidney RAS →
no compensatory mechanism → Na and water retention → “volume-dependent” or
Goldblatt HTN (Volume-Hypertensive model).


·
sustained HTN is due to:
Ø ↑
endothelin (Local paracrine effect)
Ø RAAS
activation
Ø oxidative
stress
Ø structural
changes of the heart and arteries.





